Top 5 Challenges Patients Face Interacting with Pharmaceutical Access and Reimbursement Contact Centers and What to Do About It.
When it comes to insurance coverage and financial aspects of healthcare, patients often need to reach out to access and reimbursement contact centers. These contact centers serve as valuable resources as they assist with a range of services such as verifying insurance coverage, navigating prior authorizations, addressing reimbursement inquiries, conducting benefit investigations, and providing guidance on financial resources. However, the system can be complex for patients to navigate, leading to various challenges. Understanding these challenges and implementing effective solutions can significantly improve the patient's experience and ensure access to necessary information and support throughout their treatment journey.
Top 5 Challenges Patients Face:
- Complex Terminology: Patients encounter confusing and non-inclusive terminology related to benefits investigations, insurance, department-specific acronyms, and medical terminology. This lack of familiarity with the language can create barriers and hinder understanding.
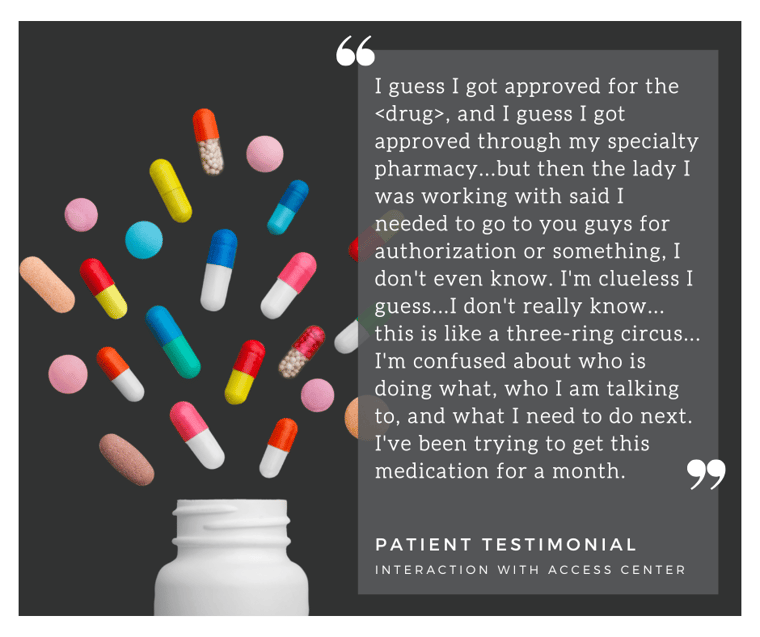
- Multiple Entities and Roles: Patients often interact with various entities such as healthcare providers, treatment sites, patient support programs, insurance companies, and specialty pharmacies. Keeping track of these parties and understanding their roles while navigating their medical challenges can be overwhelming for patients.
- Complex Insurance Processes: Insurance plans have intricate processes that patients must navigate to authorize treatment, receive support, claim payments, access copay programs, and more. These complexities can lead to delays in accessing necessary treatments and cause frustration for patients.
- Limited Awareness of Resources: Patients may struggle to access necessary resources or remain unaware of available support programs. This lack of awareness further hinders their ability to navigate the complexities of obtaining life-saving treatments.
- Financial Hardships: Despite having insurance coverage, copayments, and discount programs, many patients still face financial hardships that prevent them from obtaining or continuing their treatments. The high costs associated with treatments act as a significant barrier for patients and can lead to prescription abandonment.
 Solutions to Improve the Patient Experience:
Solutions to Improve the Patient Experience:
- Building Trust and Open Relationships: Creating a judgment-free environment where patients feel comfortable reaching out for assistance, asking questions, and addressing concerns about costs or challenges related to medication.
- Use of Plain Language: Communicating with patients in clear, easily understandable terms that cater to a sixth-grade reading level or below, ensuring accessibility for all patients.
- Providing Comprehensive Explanations: Offering thorough information and explanations of the processes involved in accessing and reimbursing medication, ensuring patients understand each step and know where to seek help when needed.
- Diverse Support Resources: Creating various support resources such as educational materials, videos, flow charts, helplines, and online portals catering to different learning styles and literacy levels. These resources can be distributed through healthcare providers, mailings, enrollment packages, or online platforms.
- Streamlining Insurance Processes: Simplifying insurance-related procedures, removing unnecessary complexities and steps, and reducing the burden on patients. Taking ownership of the process can minimize the number of interactions required to provide the necessary support.
- Proactive Exploration of Financial Assistance: Proactively informing patients about financial assistance programs, discounts, or grants that can alleviate the financial burden associated with their treatments.
- Education on Insurance Benefits: Providing comprehensive education on insurance benefits, including coverage details, limitations, and effective navigation of insurance processes.
- Promoting Accessibility: Encouraging increased accessibility and improved requirements for enrollment in patient support programs, ensuring they are more readily available and beneficial for patients in need.
To enhance the patient's experience when interacting with access and reimbursement contact centers, it is essential to adopt a patient-centered approach that prioritizes clear communication, education, and support. By utilizing plain language, providing comprehensive explanations, simplifying insurance requirements, expanding support resources, exploring financial assistance options, and educating patients about their insurance benefits, we can bring about several significant benefits for patients.
These benefits include empowering patients to take charge of their healthcare decisions, reducing confusion and frustration by demystifying complex processes, facilitating timely access to life-saving treatments, improving medication adherence, and alleviating financial burdens. Additionally, by fostering trust and open relationships, patients are more likely to reach out for assistance, enabling early intervention and proactive problem-solving.
By advocating for increased accessibility, promoting patient-centric resources, and ensuring that patient support programs are readily available and beneficial, we can create a healthcare system that better meets the needs of patients. These efforts contribute to an improved patient experience, leading to better health outcomes and enhanced overall well-being.
At Centerfirst, every day we work towards our Just Cause of living in a world where every patient's voice is clearly heard, and every patient's need is completely addressed. We understand how crucial it is to listen to the voice of your patient and continually strive to improve the patient's experience.
Are you ready to improve your patients' experience? Contact us to learn more.
