Top 7 Challenges Patients Face Interacting with Adverse Event Reporting Lines and What to Do About It
Patient confusion and uncertainty surrounding adverse event reporting present significant challenges within the healthcare system. When patients and caregivers are unexpectedly asked to report adverse events, they often find themselves unprepared, leading to confusion and potential gaps in the reporting process. These challenges are further exacerbated by communication barriers, burdensome lengthy calls, privacy concerns, unresolved issues, and a lack of trust. However, implementing focused solutions can enhance the adverse event reporting process, empowering patients to feel supported, informed, and equipped to report their experiences accurately. By addressing these challenges, healthcare organizations can improve patient engagement and ensure the integrity of adverse event reporting, ultimately enhancing patient safety and the overall quality of care.

Challenge 1: Patient Confusion and Uncertainty Regarding Adverse Event Reporting:
Patients and caregivers often experience confusion due to a lack of understanding around the adverse event intake process and its importance. This confusion may hinder their ability to effectively communicate their experiences, leading to potential gaps in reporting and an overall sense of uncertainty throughout the process.
Solutions:
- Educate patients on what constitutes an adverse event, even if it is an abstract event, and explain the importance of reporting for post-marketing safety monitoring and updates.
- Reassure patients that reporting an adverse event does not imply wrongdoing or result in any penalties, emphasizing that their well-being and safety are essential.
- Obtain patient consent, ask for any questions, and create a supportive environment before proceeding with questioning.
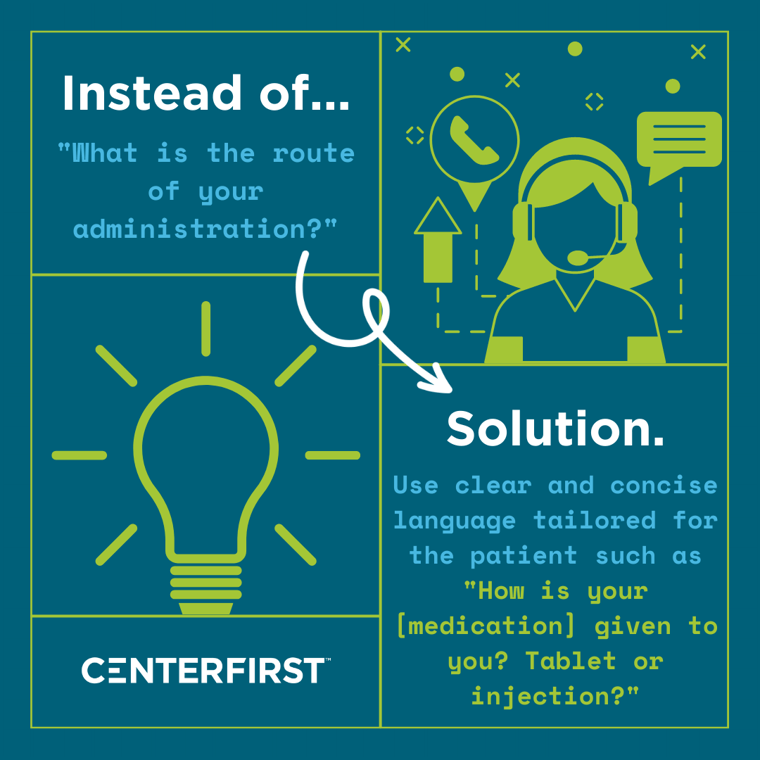
Challenge 2: Communication Barriers Due to Complex Questions and Medical Jargon:
The utilization of medical jargon in adverse event intake questions, derived from FDA (Food and Drug Administration) reporting forms, can create frustration and confusion for patients with limited health literacy. This communication barrier not only impedes accurate reporting but also contributes to a non-inclusive environment, where patients may feel excluded or overwhelmed by the technical language used.
Solutions:
- Simplify the reporting process, minimizing unnecessary complexities and making it more user-friendly for patients.
- Avoid using medical jargon, acronyms, or buzzwords that may intimidate patients and contribute to frustration or confusion.
- Frame questions in a patient-centric manner, using clear and concise language that meets patients at their level of understanding.
Challenge 3: Extensive Questioning Leading to Burdensome and Frustratingly Long Calls:
Interactions with adverse event reporting lines often result in lengthy calls, frequently exceeding 30 minutes, due to the considerable number of complex questions asked. The time-intensive nature of these calls may lead to patient fatigue and dissatisfaction, impacting their overall experience and potentially hindering their willingness to report adverse events in the future.
Solutions:
- Streamline the intake questions, distinguishing between critical and supplemental information to collect.
- Prioritize questions with a patient-centric focus, ensuring clarity and conciseness to meet patients' understanding.
- Set expectations at the beginning of the call and frequently check in with patients throughout the intake process to respect their time.
- Normalize patient feelings and emotions and demonstrate genuine empathy and compassion every step of the way.
Challenge 4: Patients Caught Unprepared for Reporting:
Patients are generally unprepared when unexpectedly asked to report an adverse event, particularly if they were transferred from another department. This situation can lead to confusion and surprise, especially when they are requested to provide information about side effects, off-label use, and personal details. The lack of preparedness can create frustration and make the reporting process more challenging for patients.
Solutions:
- Improve communication and coordination between different departments to minimize surprises for patients when they are transferred to adverse event reporting lines.
- Develop protocols and procedures to facilitate a smooth transition from other departments to adverse event reporting lines, ensuring patients receive clear explanations and understand the purpose of the reporting process.
- Provide a clear introduction to the adverse event reporting process and explain its importance at the beginning of the call.
- Acknowledge patients' potential surprise or lack of preparedness, demonstrating understanding and offering reassurance.
Challenge 5: Privacy Concerns and Perceived Invasiveness in the Reporting Process:
The adverse event reporting process can be perceived as invasive by patients when asked to share detailed and private health information. This aspect of the process raises concerns about privacy and prompts questions regarding the purpose and handling of the collected information. Patients may feel uncomfortable or hesitant to disclose sensitive details, which can create a barrier to effective reporting.
Solutions:
- Address privacy concerns by providing clear explanations about the purpose and confidentiality measures of the adverse event reporting process.
- Obtain patient consent and address any questions before delving into detailed questioning, ensuring patients feel comfortable and informed.
- Normalize patient feelings and emotions, demonstrating genuine empathy and compassion throughout the entire process.

Challenge 6: Unresolved Concerns and Lack of Benefit from Adverse Event Reporting:
Patients share detailed accounts of their side effects and medication experiences during interactions with adverse event reporting lines. However, they also often ask questions regarding these side effects and experiences that the agent is unable to answer. This lack of resolution leaves patients feeling frustrated and dissatisfied with the process. Furthermore, the reporting of adverse events often lacks tangible benefits for patients, which further reduces their motivation to participate and overall satisfaction with the reporting experience.
Solutions:
- Equip agents with the necessary resources and language to understand frequent questions asked by patients, enabling them to guide patients in finding answers.
- Foster a supportive and empathetic environment during the reporting process, ensuring patients feel comfortable and empowered to share their experiences.
- Allocate time to show gratitude, acknowledge, or affirm their valuable contribution in sharing their information for the benefit of all, while providing a clear explanation of the subsequent actions and potential outcomes.
Challenge 7: Lack of Trust and Patient-Centric Approach:
Patients perceive interactions with the adverse event reporting lines as transactional and one-sided, prioritizing data collection over addressing their needs and concerns. This lack of personal touch, empathy, and patient-centric approach leads to a feeling of being unheard and a lack of trust in the process. Consequently, the focus on completing the form can overshadow the importance of addressing the patient's individual experiences and concerns, potentially resulting in the omission of crucial information and patient dissatisfaction.
Solutions:
- Provide a clear purpose for the adverse event intake process at the beginning of each conversation, ensuring patients understand the value it provides to their specific situation and overall patient outcomes.
- Allow patients to ask questions about the process, guiding them to fully comprehend the importance and benefits of adverse event reporting.
- While agents may not answer medical questions directly, they can provide guidance and direct patients toward appropriate resources to address their inquiries, fostering a sense of resolution and minimizing a one-sided approach.
Efficient and patient-centric adverse event reporting is crucial for maintaining drug safety and patient well-being. By addressing the challenges of patient confusion, communication barriers, lengthy calls, lack of trust, and privacy concerns, pharmaceutical organizations can create a more inclusive and transparent reporting process. Through patient education, streamlined procedures, clear communication, and a supportive environment, patients can feel more prepared, empowered, and satisfied with the adverse event reporting experience. These solutions foster patient engagement, improve the quality of reported data, and contribute to the overall safety and efficacy of medications.
At Centerfirst, every day we work towards our Just Cause of living in a world where every patient's voice is clearly heard, and every patient's need is completely addressed. We understand how crucial it is to listen to the voice of your patient and continually strive to improve the patient's experience.
Are you ready to improve your patient’s experience? Contact us to learn more.
